Letter from the President
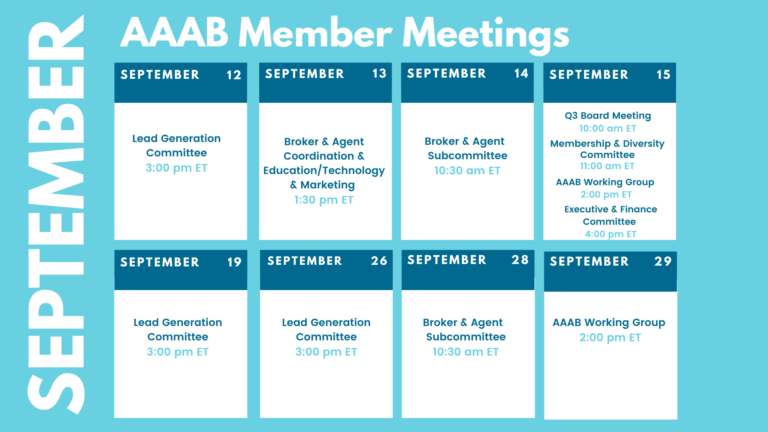
 In this issue of AAAB Insights, check out the most recent regulatory updates out of Washington D.C. and across the country in Regulatory Updates. Please make a note of the upcoming September meetings that are listed in the Members' Spot. If you would like to join a committee, please reach out and we can help you get involved.
In this issue of AAAB Insights, check out the most recent regulatory updates out of Washington D.C. and across the country in Regulatory Updates. Please make a note of the upcoming September meetings that are listed in the Members' Spot. If you would like to join a committee, please reach out and we can help you get involved.
We welcome any questions or feedback you may have regarding AAAB, so please feel free to contact our leadership board via email at gfeng@aaab.net.
Brandon Wood
AAAB President
Regulatory Updates
From DC:
ACA:
- Enhanced Subsidies Extended: As part of the Inflation Reduction Act, the Senate recently passed and the President signed a three-year extension (through 2025) of enhanced subsidies for people buying their own health coverage on the ACA Marketplaces. These temporary subsidies were originally slated to last two years (2021 and 2022) and were passed as part of the American Rescue Plan Act. The enhanced subsidies increase the amount of financial help available to those already eligible and also newly expand subsidies to middle-income people, many of whom were previously priced out of coverage.
- Preventative Care: According to NPR, the Affordable Care Act has survived many challenges in court, but the case of Kelley v. Becerra – now before a federal judge in Texas – threatens to undermine one of the most popular provisions in the law, which requires most health plans to provide coverage for preventive care with no copays. If the judge rules in favor of the plaintiffs, access to free birth control, cancer screenings, vaccines, HIV pre-exposure prophylaxis, counseling for alcohol misuse, diet counseling for people at higher risk of chronic disease, and many more preventive services would be in jeopardy, according to the nation's leading doctors' groups.
- ACA Rates Set to Fall in Virginia Next Year: Filings with the State Corporation Commission indicate that individual health insurance premiums will fall in Virginia next year, with Anthem Blue Cross Blue Shield and Cigna Health and Life Insurance Co. proposing average rate decreases of 10.5% and 19.6%, respectively. The rates must still be reviewed by the Bureau of Insurance.
- Record-High Insurance Navigator Grants: The U.S. Department of Health and Human Services announced $98.9 million for Affordable Care Act health insurance exchange navigators for the 2023 open enrollment period, which is higher than the funding provided in previous years. HHS Secretary Xavier Becerra said, "We're doubling down on our efforts to ensure people get the insurance they need. Navigators critically help us reach people where they are, educating them on their health insurance options that can be lifesaving." Centers for Medicare and Medicaid Services grants will be allocated to 59 organizations, including $12.5 million for additional efforts to help those switching from Medicaid or the Children's Health Insurance Program to exchange coverage.

Medicare/Medicaid:
- Medicaid Postpartum: Three more states have agreed to extend postpartum Medicaid coverage for up to 12 months. The U.S. Department of Health and Human Services extended additional approvals this week for Connecticut, Kansas, and Massachusetts. It is expected that these additional approvals will impact an additional 19,000 people annually.
- Medicare Beneficiaries Are More Likely to Reach Catastrophic Spending on Insulin: Among people who filled at least one insulin prescription, 14.1% reached catastrophic health spending — out-of-pocket medical spending greater than 40% of a household’s remaining income after subsistence needs are met — and almost two-thirds of them were Medicare beneficiaries, according to a recent Health Affairs study. The study was based on data from the Medical Expenditure Panel Survey in 2017 and 2018. Among the respondents who filled at least one insulin prescription, 41.1% were covered by Medicare and 35.7% by private insurance. Median annual out-of-pocket spending on insulin was $97.72, while people with Medicare coverage and private insurance paid much more than Medicaid enrollees. The research indicated that elderly patients with low family incomes were at the greatest risk for high out-of-pocket spending, and “policies that cap monthly out-of-pocket spending on insulin for Medicare beneficiaries are likely to be impactful.”
- Behavioral Health in Medicaid: Two digital health startups have teamed up to make it easier for Medicaid patients to get access to much-needed behavioral health services from their homes. Home-based healthcare technology company MedArrive is teaming up with Brave Health, a virtual-first behavioral health provider, to refer customers who need behavioral health services to Brave. Through the partnership, if MedArrive identifies an eligible health plan member in need of mental health support, MedArrive’s field providers can immediately refer that member to Brave Health’s behavioral health providers in real-time and schedule care within 72 hrs.
- Humana, Elevance Realign Business Segments, Anticipate Strong 2023 AEP: After seeing improved medical cost trends and, in some cases, lower administrative costs, Humana Inc. and Elevance Health, Inc. recently lifted their earnings projections for the full year. Conference calls to discuss second-quarter 2022 earnings were full of questions about pricing and changes related to their Medicare Advantage (MA) products as the 2023 Annual Election Period (AEP) approaches, but executives were more focused on touting efforts to serve members holistically, including through rebranding strategies as companies attempt to align their various business segments.
Federal Activity:
Federal Register: In the month of August, there were 17 new Federal register entries in the Healthcare Reform section. Those entries break down as follows:
- Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2023 and Updates to the IRF Quality Reporting Program (CMS): This final rule updates the prospective payment rates for inpatient rehabilitation facilities for the Federal fiscal year 2023.
- Medicare Program; Request for Information on Medicare (CMS): This request for information seeks input from the public regarding various aspects of the Medicare Advantage program.
- Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities; Updates to the Quality Reporting Program and Value-Based Purchasing Program for Federal Fiscal Year 2023; Changes to the Requirements for the Director of Food and Nutrition Services and Physical Environment Requirements in Long-Term Care Facilities (CMS): This final rule updates payment rates; forecast error adjustments; diagnosis code mappings; the Patient-Driven Payment Model (PDPM) parity adjustment; the SNF Quality Reporting Program (QRP); and the SNF Value-Based Purchasing (VBP) Program.
- Agency Information Collection Activities: Submission for OMB Review; Comment Request (CMS): The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
- Nondiscrimination in Health Programs and Activities (CMS): The Department of Health and Human Services (HHS or the Department) is issuing this proposed rule on Section 1557 of the Affordable Care Act (ACA) (Section 1557). Section 1557 prohibits discrimination on the basis of race, color, national origin, sex, age, or disability in certain health programs and activities.
- Agency Information Collection Activities: Proposed Collection; Comment Request (CMS): The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
- Proposed Collection; Comment Request for Affordable Care Act Internal Claims and Appeals and External Review Disclosures (IRS): The Internal Revenue Service, as part of its continuing effort to reduce paperwork and respondent burden, invites the general public and other Federal agencies to take this opportunity to comment on continuing information collections, as required by the Paperwork Reduction Act of 1995.
- Agency Information Collection Activities: Proposed Collection: Public Comment Request Information Collection Request Title: Initial and Reconciliation Application Forms to Report Graduate Medical Education Data and Full-Time Equivalent (FTE) Residents Trained by Hospitals Participating in the Children's Hospitals Graduate Medical Education Payment Program; and FTE Resident Assessment Forms to Report FTE Residents Trained by Organizations Participating in the Children's Hospitals and Teaching Health Center Graduate Medical Education Programs, OMB No. 0915-0247-Revision (HRSA): In compliance with the requirement for the opportunity for public comment on proposed data collection projects of the Paperwork Reduction Act of 1995, HRSA announces plans to submit an Information Collection Request (ICR), described below, to the Office of Management and Budget (OMB).
- Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2023 Rates; Quality Programs and Medicare Promoting Interoperability Program Requirements for Eligible Hospitals and Critical Access Hospitals; Costs Incurred for Qualified and Non-Qualified Deferred Compensation Plans; and Changes to Hospital and Critical Access Hospital Conditions of Participation (CMS): This final rule will: revise the Medicare hospital inpatient prospective payment systems for operating and capital-related costs of acute care hospitals; make changes relating to Medicare graduate medical education for teaching hospitals; update the payment policies and the annual payment rates for the Medicare prospective payment rates for the Medicare prospective payment system for inpatient hospital services provided by long-term care hospitals.
- Announcement of the Advisory Panel on Outreach and Education (APOE) September 15, 2022 Virtual Meeting (CMS): This notice announces the next meeting of the APOE (the Panel) in accordance with the Federal Advisory Committee Act.
- Securing Access to Reproductive and Other Healthcare Services (Executive Office of the President):
- Privacy Act of 1974; Matching Program (CMS): In accordance with subsection (e)(12) of the Privacy Act of 1974, as amended, the Department of Health and Human Services (HHS), Centers for Medicare & Medicaid Services (CMS) is providing notice of a new matching program between CMS and the Department of the Treasury (Treasury), Internal Revenue Service (IRS).
- Medicaid Program and CHIP; Mandatory Medicaid and Children's Health Insurance Program (CHIP) Core Set Reporting (CMS): This proposed rule would establish the requirements for mandatory annual State reporting of the Core Set of Children's Health Care Quality Measures for Medicaid and Children's Health Insurance Program (CHIP), the behavioral health measures on the Core Set of Adult Health Care Quality Measures for Medicaid, and the Core Sets of Health Home Quality Measures for Medicaid.
- Agency Information Collection Activities: Submission for OMB Review; Comment Request (CMS): The Centers for Medicare & Medicaid Services is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
- Advisory Committee on Immunization Practices (CMS): In accordance with the Federal Advisory Committee Act, the Centers for Disease Control and Prevention (CDC), located within the Department of Health and Human Services (HHS), announces the following meeting of the Advisory Committee on Immunization Practices.
- Deferred Action for Childhood Arrivals (DHS): On September 28, 2021, the Department of Homeland Security published a notice of proposed rulemaking that proposed to establish regulations to preserve and fortify the Deferred Action for Childhood Arrivals policy to defer removal of certain noncitizens who years earlier came to the United States as children.
- SES Positions That Were Career Reserved During CY 2019 (OPM): This gives notice of all positions in the Senior Executive Service (SES) that were career reserved during calendar year 2019.
Bills Introduced in Key Health Committees:
- House Energy & Commerce: 35 bills were introduced in August. None involving ancillary products.
- House Ways & Means: 28 bills were introduced in August. One of interest to the AAAB is the “Chiropractic Act of 2022” which ensures equitable treatment of items and services furnished by chiropractors under the Medicare program came out on August 12th.
- Senate Finance: 16 bills were introduced in August. One of interest to the AAAB is the “The Occupational Therapy Mental Health Parity Act” which will provide education and outreach to stakeholders about the Medicare Benefit Policy Manual with respect to occupational therapy services furnished to individuals under the Medicare program for the treatment of substance use or mental health disorder diagnosis using applicable Healthcare Common Procedure Coding System (HCPCS) codes.
- Senate HELP: 9 bills were introduced in August. One of interest to the AAAB is the “Increasing Access to Dental Insurance Act” which increases access from the Affordable Care Act.
Salient Congressional Bills:
- HR 4803-Acupuncture for Our Seniors Act: Facilitates access to acupuncture in the Medicare program.
- HR 7512-Protecting Patients from Deceptive Health Plans Act: Limits the sale of supplemental products to consumers who already have comprehensive coverage. Would disallow the combination of accident and disability coverage. Currently in committee.
- S 1002-Junk Plan Accountability and Disclosure Act of 2021: Would require pre-enrollment disclosures by insurers selling supplemental plans. Significant federal reporting requirements on enrollment and claims. Currently in committee.

Around the Country:
- Cerner Layoffs: Oracle has begun cutting U.S. jobs with workforce reductions primarily impacting marketing and customer experience divisions, according to media reports. Posts on Reddit and thelayoff.com indicate that the workforce reduction is impacting Cerner as well.
- Humana Earnings: Humana Inc. delivered robust financial results in the second quarter of 2020, with earnings far outstripping the Wall Street consensus. The Medicare Advantage-focused insurer credited lower-than-expected utilization for the strong result, provided investors with more detail about its plans to reorganize following several notable provider transactions, and touted plans to expand its Medicaid business.
- Telehealth: Telehealth Company Amwell is working with CVS Health to roll out the retail drugstore giant’s new virtual primary care service. CVS announced at the end of May plans to launch a virtual care service that gives consumers access to primary care, on-demand care, chronic condition management, and mental health services. CVS virtual care platform is a consumer-centric offering designed to bring together the many elements of the CVS Health system into a single integrated experience.
- Nurses Strike: More than 15,000 Minnesota nurses have signed off on strikes at 15 hospitals across seven different health systems over issues of short-staffing, retention and patient safety.
- Amazon Care is shutting down at the end of 2022: Three years after it began piloting a primary care service for its employees that blended telehealth and in-person medical services, Amazon plans to cease operations of its Amazon Care service for employers.
- FDA Approves Gene Therapy Drug Priced at Record $2.8 Million: After the FDA approved Zynteglo (betibeglogene autotemcel) on Aug. 17 for the treatment of transfusion-dependent beta-thalassemia, the gene therapy’s manufacturer, bluebird bio, Inc., announced the drug would have a $2.8 million wholesale acquisition cost (WAC). That is the highest WAC for a drug hitting the market in the U.S.
Members' Spot
Upcoming Member Opportunities
Get involved! If you aren't currently serving on a committee, but would like to, please email gfeng@aaab.net.
Hear From AAAB