Letter from the President
 Summer is here and health care is heating up. In the June issue of AAAB Insights, check out the most recent regulatory updates out of Washington D.C. and across the country in Regulatory Updates.
Summer is here and health care is heating up. In the June issue of AAAB Insights, check out the most recent regulatory updates out of Washington D.C. and across the country in Regulatory Updates.
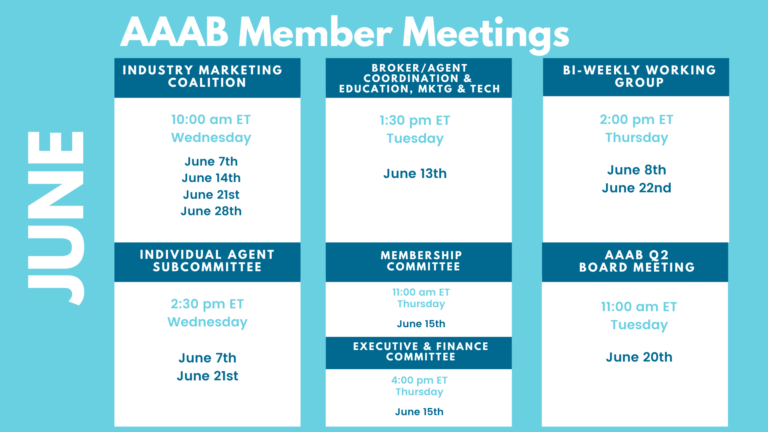
Please make a note of the upcoming May meetings that are listed in the Members' Spot. If you would like to join a committee, please reach out to get involved.
We welcome any questions or feedback you may have regarding AAAB, so please feel free to contact our leadership board via email at gfeng@aaab.net.
Brandon Wood
AAAB President
Regulatory Updates

From DC:
ACA:
- Friday Health Plans Suspended in North Carolina: North Carolina is suspending any new enrollment in plans offered by Friday Health Plans Inc., a Texas-based health insurance startup. New members will not be able to enroll in Friday Health Plans for the remainder of 2023, but coverage will remain unchanged for current members. In recent weeks, the startup has also been placed under receivership by the Texas Department of Insurance and ordered to liquidate. The company launched in 2015 and focused on marketplace products, later expanding to Individual Coverage Health Reimbursement Arrangements (ICHRAs). However, like other startups, it struggled to reach profitability or substantial market share. Prior to its Texas receivership, Friday enrolled 381,691 members in seven states.
- Georgia Moving to State-based Exchange: Georgia Gov. Brian Kemp (R) recently signed into law a bill that establishes a state-run Affordable Care Act exchange, moving the state away from the federal marketplace. CMS must still approve of the transition, which would begin this fall for coverage beginning in January 2024. The three largest exchange insurers in Georgia are Centene Corp. with 325,239 members, Elevance Health with about 70,000 members, and Oscar Health with about 70,000 members.
- ACA in Court: The Fifth Circuit Court ruled recently in favor of an administrative stay while it reviews the case. Texas Judge Reed O'Connor ruled in March that the federal government could not enforce preventive care mandates under the ACA, which require payers to cover a slew of services at no cost. The initial lawsuit centered on birth control and pre-exposure prophylaxis (PrEP) drugs, which prevent HIV infections. O'Connor ruled last fall that requiring Christian-owned companies to cover these products violated their religious rights, and the March ruling aims to eliminate preventive care mandates broadly.
Medicare/Medicaid:
- Big Blue Boxes: In the first year of the COVID-19 pandemic, when many people were having trouble accessing basic personal protective equipment, Highmark Blue Cross Blue Shield began sending out care kits including PPE and other items to support seniors at home. The response from Medicare Advantage members was so positive that what started out as a feel-good gesture has become a full-blown supplemental benefit, and the insurer continues to refine the kits to meet members’ evolving needs and ensure continued satisfaction with the plan. Starting with the plan year 2022, eligible Highmark members were given the option to receive one of 17 condition care kits. Commonly referred to as the “big blue box,” each kit is filled with a variety of items tailored to a specific condition, with a focus on member choice and high quality, speakers from Highmark and its strategic partner RR Donnelley explained during the 14th Annual Medicare Market Innovations Forum, held on March 28 and 29 in Orlando. Highmark worked with RR Donnelley on everything from the package’s contents and design to member outreach and fulfillment, and the insurer consulted clinicians to make sure the items were appropriate for each condition. For example, a telemedicine kit helps patients prepare for a virtual visit by arming them with things like a digital thermometer, blood pressure cuff and a digital floor scale. A diabetes prevention kit may contain a food scale, a cookbook, measuring cups, a portion plate, a pedometer, a fitness tracker and a fitness band, while a smoking cessation kit would include chewing gum, candy, a toothbrush, floss and a fidget toy.
- Eli Lilly Pays for Medicaid Rebate Issue: When a federal jury last year ordered Eli Lilly to pay $61 million for skimping out on Medicaid rebates, the company vowed to fight the verdict. But instead of the result Lilly wanted, the award has been tripled to more than $183 million. On Tuesday, Illinois federal judge Harry Leinenweber ruled that Eli Lilly owes triple damages from last year's award after whistleblower Ronald Streck convinced a jury that the company violated the False Claims Act and short-changed Medicaid on rebate payments.
- Better Days for MA Insuretechs: Still intent on standing apart from established Medicare Advantage competitors with their use of technology, Medicare-focused “insuretechs,” Alignment Healthcare, Inc. and Clover Health Investments Corp. recently reported first-quarter 2023 earnings that showed shrinking losses and increasing insurance revenue.
Federal Activity:
Federal Register: In the month of May, there were 15 new Federal Register entries in the Healthcare Reform section. Those entries break down as follows:
- Medicaid Program; Misclassification of Drugs, Program Administration and Program Integrity Updates Under the Medicaid Drug Rebate Program (CMS): This proposed rule would seek to implement policies in the Medicaid Drug Rebate Program (MDRP) related to the new legislative requirements in the Medicaid Services Investment and Accountability Act of 2019 (MSIAA), which are needed to address drug misclassification, as well as drug pricing and product data misreporting by manufacturers.
- National Committee on Vital and Health Statistics Meeting (HHS): Pursuant to the Federal Advisory Committee Act, the Department of Health and Human Services (HHS) announces the following advisory committee meeting. This meeting is open to the public. The public is welcome to obtain the link to attend this meeting by following the instructions posted on the Committee website: https://ncvhs.hhs.gov/.
- Agency Information Collection Activities: Proposed Collection; Comment Request (CMS): The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public. Under the Paperwork Reduction Act of 1995 (the PRA), Federal agencies are required to publish notice in the Federal Register concerning each proposed collection of information.
- Assistance to States for the Education of Children With Disabilities (ED): The Secretary proposes to amend regulations under Part B of the Individuals with Disabilities Education Act (Part B of IDEA or the Act) that govern the Assistance to States for the Education of Children with Disabilities program, including the Preschool Grants program. Specifically, the Secretary proposes to amend the IDEA Part B regulations.
- Agency Information Collection Activities: Proposed Collection; Comment Request (CMS): The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public. Under the Paperwork Reduction Act of 1995 (the PRA), Federal agencies are required to publish notice in the Federal Register concerning each proposed collection of information.
- Assistance to States for the Education of Children With Disabilities (Education Department): The Secretary proposes to amend regulations under Part B of the Individuals with Disabilities Education Act (Part B of IDEA or the Act) that govern the Assistance to States for the Education of Children with Disabilities program, including the Preschool Grants program. Specifically, the Secretary proposes to amend the IDEA Part B regulations.
- National Women's Health Week, 2023 (EOP):
- National Indian Health Outreach and Education (IHS):
- Advisory Committee on Immunization Practices (CDC): In accordance with regulatory provisions, the Centers for Disease Control and Prevention (CDC) announces the following meeting for the Advisory Committee on Immunization Practices (ACIP). This meeting is open to the public. Time will be available for public comment.
- Agency Information Collection Activities: Submission for OMB Review; Comment Request (CMS): The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public. Under the Paperwork Reduction Act of 1995 (PRA), federal agencies are required to publish notice in the Federal Register concerning each proposed collection of information.
- Intent To Award a Single-Source Supplement To Provide the National Aging Network With Timely, Relevant, High-Quality Opportunities To Further Enhance Training and Technical Assistance, Visibility, and Cultural Adaptions Related to Chronic Disease Self-Management Education (CDSME) Programs (CLA): The Administration for Community Living (ACL) announces the intent to award a single-source supplement to the current cooperative agreement held by the National Council on Aging (NCOA) for the Chronic Disease Self-Management Education (CDSME) Resource Center. The purpose of this program is to leverage and expand upon chronic disease.
- Medicaid Program; Ensuring Access to Medicaid Services (CMS): This proposed rule takes a comprehensive approach to improving access to care, quality and health outcomes, and better addressing health equity issues in the Medicaid program across fee-for-service (FFS), managed care delivery systems, and in home and community-based services (HCBS) programs. These proposed improvements seek to increase.
- Medicaid Program; Medicaid and Children's Health Insurance Program (CHIP) Managed Care Access, Finance, and Quality (CMS): This proposed rule would advance CMS' efforts to improve access to care, quality and health outcomes, and better address health equity issues for Medicaid and Children's Health Insurance Program (CHIP) managed care enrollees. The proposed rule would specifically address standards for timely access to care and States' monitoring and enforcement.
- Workers Memorial Day, May 2, 2023 (Executive Office of the President)
- Medicare Program; Proposed Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Policy Changes and Fiscal Year 2024 Rates; Quality Programs and Medicare Promoting Interoperability Program Requirements for Eligible Hospitals and Critical Access Hospitals; Rural Emergency Hospital and Physician-Owned Hospital Requirements; and Provider and Supplier Disclosure of Ownership (CMS): This proposed rule would: revise the Medicare hospital inpatient prospective payment systems (IPPS) for operating and capital- related costs of acute care hospitals; make changes relating to Medicare graduate medical education (GME) for teaching hospitals; update the payment policies and the annual payment rates for the Medicare prospective.
Bills Introduced in Key Health Committees:
- House Energy & Commerce: 131 bills filed in May–NOTABLE: H.R.3004 — To amend the Internal Revenue Code of 1986 to provide for a temporary expansion of health insurance premium tax credits for certain low-income populations, and to amend title XIX of the Social Security Act to establish a Federal Medicaid program. Sponsor: Fletcher, Lizzie [Rep.-D-TX-7].
- House Ways & Means: 75 bills filed in May–NOTABLE: None.
- Senate Finance: 33 bills filed in May–NOTABLE: S.1450 — A bill to establish a cap on costs for covered prescription drugs under Medicare parts B and D. Sponsor: Sanders, Bernard [Sen.-I-VT]. S.1592 — A bill to clarify coverage of occupational therapy under the Medicare program. Sponsor: Hassan, Margaret Wood [Sen.-D-NH]. S.1655 — A bill to establish a Medicare-for-all national health insurance program. Sponsor: Sanders, Bernard [Sen.-I-VT].
- Senate HELP: 48 bills filed in May–NOTABLE: S.1424 — 118th Congress A bill to amend title XXVII of the Public Health Service Act to improve health care coverage under vision and dental plans, and for other purposes. Sponsor: Manchin, Joe, III [Sen.-D-WV].
Salient Congressional Bills:
- H.R.711 — To amend title XXVII of the Public Health Service Act to eliminate the short-term limited duration insurance exemption with respect to individual health insurance coverage.
- H.R.1610/S.799 — To amend title XVIII of the Social Security Act to provide Medicare coverage for all physicians' services furnished by doctors of chiropractic within the scope of their license, and for other purposes.
- H.R.824 — Telehealth Benefit Expansion For Workers Act.
- H.R.3133 — To amend title XVIII of the Social Security Act to provide coverage for acupuncturist services under the Medicare program.

Around the Country:
- Kreidler Retiring: Washington State Insurance Commissioner Mike Kreidler sent an email to agency staff confirming that he will not seek reelection. "Serving alongside you as Insurance Commissioner for Washington state has been, and continues to be, the greatest honor of my life," said Kreidler. "I've always said it was the best job I've ever had, and I still feel that way today. The list of issues we've tackled could go on and on, but at the end of the day, I think of the individual people we help — the thousands of families we've advocated for, day after day. That, above all else, is what makes me the most proud of this agency and of all of you. Now, it's time for someone else to step forward and carry on this agency's important consumer protection work. I know that my successor will be in good hands with all of you helping to lead the way."
- PBM Pressure: PBMs are on the hot seat, and Express Scripts unveiled a slew of new programs aimed at addressing critics. Cigna CEO David Cordani said those initiatives have been in the works for nearly two years.
- Hospital Bailout: California lawmakers fast-tracked legislation to loan out $150 million to hospitals across the state struggling to stay open, with promises of more support to come. The state's hospital association said the loans will be a lifeline for hospitals that are "right on the edge of disaster."
- Weight Loss Drug: A growing roster of digital health companies now offer access to next-generation weight loss drugs, seeing the potential of a $100 billion market. But doctors caution that prescribing drugs without the right medical care will not help address the country's growing obesity epidemic.
- Michigan and Vermont Blues Team Up: Blue Cross Blue Shield of Michigan and Blue Cross and Blue Shield of Vermont, the largest health insurers in their respective states, have struck an agreement that will see the Vermont Blues plan become a subsidiary of BCBS of Michigan. The nonprofit companies said in a May 1 news release that this deal “is an affiliation, not an acquisition, which means there is no financial exchange between the organizations.”
- For-profit Hospitals More Generous: In testimony in front of the House Committee on Ways and Means on the efficacy of nonprofit hospitals, Johns Hopkins University professor and CBO health policy advisor Dr. Ge Bai said that for-profit hospitals provide more charity care than non-profits. Bai discussed the failure of many nonprofit hospitals to provide community benefit, noting that nonprofit hospitals increasingly provide less charity care than for-profit hospitals. According to Bai, “In aggregate, tax-exempt hospitals spent $2.30 of every $100 in total expenses incurred on charity care, which was less than for-profit hospitals ($3.80). More than one-third of tax-exempt hospitals (36%) provided less than $1 of charity care for every $100 in total expenses.”
Members' Spot
Upcoming Member Opportunities
Get involved! If you aren't currently serving on a committee, but would like to, please email gfeng@aaab.net.