Letter from the President
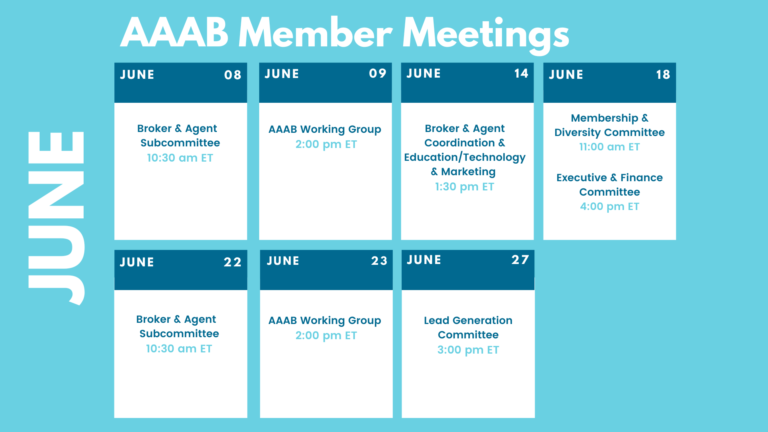
 In this issue of AAAB Insights, check out the most recent regulatory updates out of Washington D.C. and across the country in Regulatory Updates and information from our most recent member committee meetings in Committee Updates. Please make a note of the upcoming June meetings that are listed in the Members' Spot. If you would like to join a committee, please reach out and we can help you get involved.
In this issue of AAAB Insights, check out the most recent regulatory updates out of Washington D.C. and across the country in Regulatory Updates and information from our most recent member committee meetings in Committee Updates. Please make a note of the upcoming June meetings that are listed in the Members' Spot. If you would like to join a committee, please reach out and we can help you get involved.
We welcome any questions or feedback you may have regarding AAAB, so please feel free to contact our leadership board via email at gfeng@aaab.net.
Brandon Wood
AAAB President
Regulatory Updates
From DC:
ACA:
- ACA Insurer Fined: In an interview with the Denver Gazette, Colorado Division of Insurance Commissioner Michael Conway said he nearly banned Bright Health from operating in the state, and would have forced an immediate shut-down fueled by member and provider complaints. Instead, the division fined the startup $1 million. Bright Health is the second-largest individual insurer in Colorado, with 61,423 members.
- Senators Call Out IRS: On May 11, Ranking Member of the Senate HELP Committee, Senator Richard Burr, with Senators Bill Cassidy and Pat Toomey sent a letter to IRS Commissioner Charles Rettig saying the “family glitch” fix was illegal. This so-called “family glitch” fix was proposed in a rule the previous month. From their letter: “The IRS has no constitutional basis for unilaterally changing the laws Congress has enacted, and the American people must have confidence that their tax collector is not unilaterally imposing its will onto them.”
- Georgia Blocked: On April 29, CMS blocked Georgia from moving away from using the federal ACA marketplace exchange through HealthCare.gov and creating its own model. The new Georgia model was approved in November 2020 under the previous Administration and would have required marketplace customers to purchase health insurance directly from insurers or web brokers instead of HealthCare.gov, which the state currently uses. In a letter to the director of the Georgia Office of Health Strategy and Coordination, CMS Administrator Chiquita Brooks-LaSure stated that CMS’ decision to not allow Georgia to end using the federal exchange was due to two findings: (1) Georgia failed to comply with its section 1332 waiver’s specific terms and conditions by repeatedly not providing HHS and the Treasury Department with requested information as part of their oversight and monitoring authority, and (2) the Georgia section 1332 waiver no longer met the statutory guardrails that it will provide coverage to at least a comparable number of residents as without the waiver.
Medicare:
- CMS Finalizes MA Rule: Just a month shy of the bid deadline for the 2023 plan year, CMS on April 29 finalized most provisions of a sweeping Medicare Advantage and Part D rule that was proposed in January. Those provisions included restoring detailed medical loss ratio (MLR) reporting requirements, requiring MA Special Needs Plans to incorporate certain questions on social risk factors into health risk assessments, and finalizing a pathway to allow for star ratings to reflect a Dual Eligible SNP’s local performance. However, one proposed Part D provision regarding pharmacy direct and indirect remuneration (DIR) was notably delayed, allowing plans, pharmacies and pharmacy benefit managers time to renegotiate pharmacy pacts.
- Federal Task Force: The American Hospital Association wants the federal government to launch a series of probes into commercial payers that routinely deny access to care and services. The hospital group wrote to the Department of Justice recently pressing for False Claims Act investigations after a recent report from a federal watchdog found some Medicare Advantage plans have used prior authorization to deny care in violation of Medicare coverage rules. The agency also pressed the Centers for Medicare & Medicaid Services to weigh in.
- Ohio is THE Medicare Advantage State: According to new research from the Kaiser Family Foundation, 14 of the 25 counties that offered the most Medicare Advantage plans in 2022 were located in Ohio. The county with the single most offerings was Ohio’s Summit County, with 82 plan choices. Ohio has the sixth-largest Medicare Advantage population in the U.S., with 1,246,706 members. Anthem, Inc., leads the Ohio market, with 315,684 enrollees.

Federal Regulations:
In the month of June, there were 15 new Federal register entries in the Healthcare Reform section. Those entries break down as follows:
- SES Positions That Were Career Reserved During CY 2021 (PMO): This is a notice of all positions in the Senior Executive Service (SES) that were career reserved during calendar year 2021.
- Agency Information Collection Activities: Submission for OMB Review; Comment Request (CMS): CMS is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
- Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2023 (HHS): This final rule includes payment parameters and provisions related to the risk adjustment and risk adjustment data validation programs, as well as 2023 user fee rates for issuers offering qualified health plans through Federally-facilitated Exchanges and State-based Exchanges on the Federal platform.
- Medicare Program; Contract Year 2023 Policy and Technical Changes to the Medicare Advantage and Medicare Prescription Drug Benefit Programs; Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency; Additional Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency (CMS): This final rule will revise the Medicare Advantage program and Medicare Prescription Drug Benefit program regulations to implement changes related to marketing and communications, past performance, Star Ratings, network adequacy, medical loss ratio reporting, special requirements during disasters or public emergencies, and pharmacy price concessions.
- Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Proposed Policy Changes and Fiscal Year 2023 Rates; Quality Programs and Medicare Promoting Interoperability Program Requirements for Eligible Hospitals and Critical Access Hospitals; Costs Incurred for Qualified and Non-Qualified Deferred Compensation Plans; and Changes to Hospital and Critical Access Hospital Conditions of Participation (CMS): This proposed rule would: Revise the Medicare hospital inpatient prospective payment systems for operating and capital-related costs of acute care hospitals; make changes relating to Medicare graduate medical education for teaching hospitals; update the payment policies and the annual payment rates for the Medicare prospective payment system (PPS) for inpatient hospital services provided by long-term care hospitals.
- World Trade Center Health Program; Addition of Uterine Cancer to the List of WTC-Related Health Conditions (HHS): Title I of the James Zadroga 9/11 Health and Compensation Act of 2010 amended the Public Health Service Act to establish the World Trade Center Health Program. The WTC Health Program, which is administered by the Director of the National Institute for Occupational Safety and Health, within CDC, provides medical monitoring and treatment to eligible responders to the September 11, 2001, terrorist attacks in New York City, at the Pentagon, and in Shanksville, Pennsylvania, and to eligible survivors of the New York City attacks.
- Advisory Committee on Immunization Practices (CDC): In accordance with the Federal Advisory Committee Act, the Centers for Disease Control and Prevention announces the following meeting of the Advisory Committee on Immunization Practices. This meeting is open to the public. Time will be available for public comment.
- Announcing the Intent To Award a Single-Source Supplement for the National Center for Benefits Outreach and Enrollment (Community Living Administration): The Administration for Community Living announces the intent to award a single-source supplemental to the current cooperative agreement held by the National Council on Aging or the National Center for Benefits Outreach and Enrollment.
- National Women's Health Week, 2022 (Executive Office of the President): A Proclamation–"During National Women's Health Week, we recommit to ensuring the health and well-being of women and girls across our Nation. …"
- National Committee on Vital and Health Statistics (HHS): Pursuant to the Federal Advisory Committee Act, the Department of Health and Human Services announces the following advisory committee meeting.
- Basic Health Program; Federal Funding Methodology for Program Year 2023 and Proposed Changes to Basic Health Program Regulations (CMS): This document proposes the methodology and data sources necessary to determine Federal payment amounts to be made for program year 2023 to States that elect to establish a Basic Health Program under the Patient Protection and Affordable Care Act to offer health benefits coverage to low-income individuals otherwise eligible to purchase coverage through Health Insurance Exchanges.
- Agency Information Collection Activities: Submission for OMB Review; Comment Request (CMS): The Centers for Medicare & Medicaid Services is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
- Agency Information Collection Activities: Proposed Collection; Comment Request (CMS): The Centers for Medicare & Medicaid Services (CMS) is announcing an opportunity for the public to comment on CMS' intention to collect information from the public.
- Withdrawing Rule on Securing Updated and Necessary Statutory Evaluations Timely (FDA/PHS/CMS/CFA): The Department of Health and Human Services (HHS or Department) is issuing a final rule withdrawing a rule entitled ``Securing Updated and Necessary Statutory Evaluations Timely'' (SUNSET final rule), which published in the Federal Register of January 19, 2021.
- Privacy Act of 1974; System of Records (DOD): In accordance with the Privacy Act of 1974, the DoD is modifying and reissuing a current system of records titled, “Defense Enrollment Eligibility Reporting Systems (DEERS),” DMDC 02 DoD.
Around the Country:
- Drug Price Controls: Democratic lawmakers are expected to make a strong push to revive a variety of drug pricing proposals, such as those that would grant CMS the ability to negotiate the price of certain drugs and place a cap on Medicare beneficiaries out-of-pocket spending. Senate Majority Leader Chuck Schumer (D-N.Y.) has indicated he is targeting the current congressional work period that runs through Memorial Day as the time to make good on drug pricing plans that Democrats have long favored, noted Avalere Health.
- Drug Partnership Scrapped: According to AIS, Bristol Myers Squibb and Nektar Therapeutics are scrapping their $2 billion partnership. The companies were testing combinations of Opdivo and bempegaldesleukin, an experimental Nektar drug designed to stimulate interleukins. The combo showed poor results in melanoma, renal cell carcinoma and urothelial cancer.
- Virtual Physical Therapy: According to Fierce Health, UnitedHealthcare has partnered with Kaia Health on a new virtual physical therapy program. The program aims to offer 24/7, on-demand exercise feedback to eligible members with musculoskeletal conditions. Members who are recovering from surgery or an injury will be asked to complete an assessment of current issues and will be referred to the program based on that assessment. Eligible members will then be able to download Kaia's app to access its physical therapy tools, which use artificial intelligence to support patients through physical therapy exercise and monitor progress.
- Centene Plans to Sell Pharmacy Businesses: Centene Corp. has agreed to sell two of its pharmacy businesses, Magellan Rx and PANTHERx Rare, in separate transactions as part of the insurer’s decision last year to exit the PBM industry. Centene purchased both companies within the past 18 months, and industry experts told AIS Health that the relatively quick sales mean the company’s management team is focusing on its core businesses and also cite lawsuits against Centene’s PBM subsidiaries.
- Insurer Pulling Out: Oscar Health announced in its first-quarter earnings call that it will be pulling out of two states, Colorado and Arkansas citing regulatory changes and slow member growth. Leadership noted that the move would not have a meaningful effect on profits. Oscar’s first quarter saw a net loss of $77 million, an improvement from an $88 million loss the year prior. The move follows a similar action by competitor Bright Health which last month announced it was exiting six states in an effort to stabilize finances.
- Commercial Costs Over Medicare: In a Rand study funded by the Robert Wood Johnson Foundation, employers and private insurers paid 224% of what Medicare would pay for the same services at the same facilities across all hospital inpatient and outpatient services on average in 2020. Researchers found significant variations in those prices across states. The American Hospital Association pushed back on the findings saying the variation in the cost of delivering services across the wide range of U.S. hospitals is expected.
Committee Updates
Committee Updates:
- Broker Committee: The committee completed the compliance toolbox and is providing it to all industry members to benefit their respective compliance programs.
- Independent Agent Subcommittee: It continues working on the the buildout of an associate and individual agent offering for the association. A significant new task is build out of a marketing plan to grow these membership offerings.
- Membership/Diversity/Product Committee: The committee continues reviewing recommendations and leads for new industry members.
Members' Spot
Upcoming Member Opportunities
Get involved! If you aren't currently serving on a committee, but would like to, please email gfeng@aaab.net.